What is a Retinal Detachment?
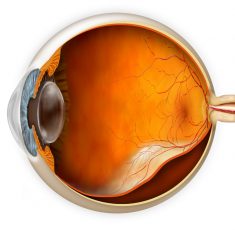
A Retinal Detachment occurs when the inner layers of the retina separate from the underlying supportive tissue that provides its oxygen and nutrients.
The retina is the curved back layer of the eye covered in light-sensitive cells that are responsible for sending visual information to the brain, and it cannot function when not in contact with the underlying support layers.
A retinal detachment is an ocular emergency as it can rapidly cause permanent vision loss.
You should seek urgent medical attention.
Eye Specialist Institute provides access to ophthalmic care for emergency after-hours and weekend appointments.
You can contact us on 1800 RETINA (1800 738 462).
Symptoms of a Retinal Detachment
The impact on a person’s eyesight depends on the location and severity of the detachment and symptoms can include:
- Sudden onset of new floaters often (dark dots, specks, cobwebs, or squiggly lines) in vision
- Bright flashing lights or sparks (like lightning or a camera flash) in your side vision
- Dark shadow or grey curtain obscuring your side vision
- Blurred or decreased vision
- Complete and sudden loss of vision
What causes a Retinal Detachment?
In most cases, retinal detachments are caused by a tear or hole in the retina which has allowed fluid to leak in between the layers of tissue, gradually separating them until a detachment occurs.
Retinal tears mostly occur due to a Posterior Vitreous Detachment, which is a normal part of ageing, however most PVDs do not result in a retinal detachment. Another cause is a trauma injury to the eye.
Find out if you are at risk below.
Am I at risk of a Retinal Detachment?
A retinal detachment can happen at any age, but it is more prevalent over the age of 60.
Other factors that may increase likelihood include:
- Posterior Vitreous Detachment (PVD)
- Short-sightedness (myopia)
- History of retinal detachment
- Genetics / Family history
- Injury or trauma to eye or face
- Eye diseases and systemic diseases (e.g. diabetic retinopathy)
Treatment of a Retinal Detachment
The aim of surgery is to halt the progression of vision loss by reattaching the retina to the back of the eye.
A retinal detachment will not get better without surgical treatment.
The type of surgery recommended by your Ophthalmologist is a complex decision that will depend on the cause, location, and type of your detachment as well as any existing eye conditions.
Vitrectomy Surgery – involves intraocular microsurgery to remove the vitreous gel of the eye and a gas bubble or silicone oil is injected into the eye to smooth the retina back into place. If a silicone oil is used, it is removed a few months later by your Ophthalmologist.
Scleral Buckle Surgery – performed under anaesthetic and involves attaching a tiny piece of silicone material to the outside of your eye to push the supportive tissue (Retinal Pigment Epithelium (RPE)), back towards the detached retina. Cryotherapy (freezing) or laser is then used to create a seal any tears or breaks in the retina.
Generally, the sooner the retina is reattached, the better the chances that vision can be maintained or restored. However, the extent to which your vision improves will depend upon how extensive the detachment was, any pre-existing eye conditions, and if your macula was detached for weeks rather than a few days.