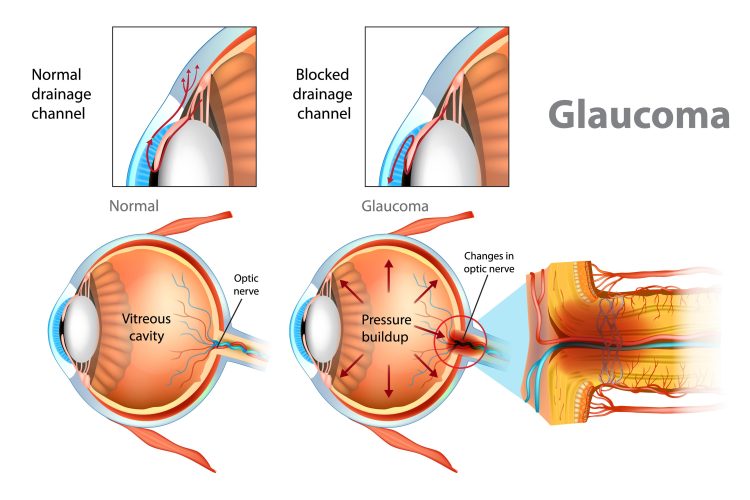
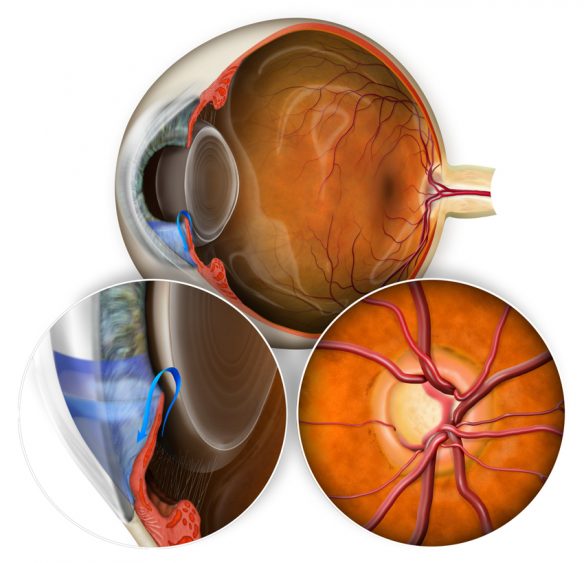
Glaucoma is the term for a group of eye diseases which cause vision loss because of damage to the optic nerve at the back of your eye, usually related to raised intraocular pressure (IOP). There are many types of glaucoma, named according to the cause of the raised IOP.
Read more about primary open-angle, angle-closure, normal-tension, secondary, congenital (childhood) and other types of glaucoma below.
Primary Open-Angle Glaucoma
The most common form of glaucoma, accounting for at least 90% of all cases, is also known as “chronic glaucoma”.
This type of glaucoma is caused by the progressive build-up of pressure inside the eyeball despite the drainage angle being open.
The angle is where your iris (the coloured part of your eye) meets your cornea (the clear front cover of eye), containing the trabecular meshwork and parts of the iris, which form the drainage system for the aqueous humour. “Open” means that on specialised testing (gonioscopy), the angle appears to be as wide as it should be and there is no physical closure of the angle.
This type of glaucoma often develops progressively and unnoticed as there are no early symptoms.
Angle-Closure Glaucoma
This type of glaucoma can be a medical emergency and urgent treatment is required to prevent significant vision loss or blindness.
This less common form of glaucoma is caused by a rapid increase in intraocular pressure due to a closure of the drainage angle, which physically prevents fluid from draining away.
This can produce symptoms including rapid vision blur, haloes around lights, eye pain, redness, nausea, vomiting, and/or severe headache.
Urgent medical attention is required to prevent significant vision loss or blindness.
Treatments differ from open angle glaucoma and requires urgent reduction of IOP with oral or intravenous diuretics, laser surgery to open up the drain (peripheral iridotomy) and in some cases, may require cataract surgery.
Normal-Tension Glaucoma
In this type of glaucoma, also known as normal pressure glaucoma or low-tension glaucoma, the optic nerve is damaged even though your intraocular pressure (IOP) is not above the normal range.
Normal-tension glaucoma is thought to develop due to individual underlying optic nerve susceptibility to even a moderate pressure or poor blood supply to optic nerve. The other risk factors include: family history of glaucoma, over 40, diabetes, history of migraines or Raynaud’s phenomenon, and African or Asian descent.
Normal-tension glaucoma can be diagnosed by observing the optic nerve for signs of damage, monitoring changes in visual field tests and managed similarly to open angle glaucoma.
Secondary Glaucoma
This type of glaucoma is when another eye condition or disease leads to the development of glaucoma.
Many eye conditions can lead to Secondary Glaucoma, including recurrent infection or inflammation in the eye, prolonged course of cortisone (steroid) medication, eye trauma, dense cataracts, some eye surgeries, severe proliferative diabetic retinopathy, retinal vein occlusion, or chronic hypoperfusion to the eyes.
The symptoms and treatments differ by the cause of the glaucoma and would usually require treatment of these underlying cause or causes, in addition to managing the raised IOP.
Congenital (Childhood) Glaucoma
This type of glaucoma occurs in children under 2 years old and is a rare condition that is caused by incorrect or incomplete development of the eye’s drainage system before birth.
Symptoms include enlarged eyes (buphthalmos), cloudiness of the cornea, watery eyes, and sensitivity to light/glare (photophobia).
Congenital glaucoma is usually detected and managed by a paediatric ophthalmologist and require specialised treatments and lifelong management of the complications from the disease.
Other Types of Glaucoma
There are other variations of glaucoma including pseudoexfoliation syndrome, pigment dispersion syndrome and glaucoma associated with Sturge Weber syndrome (port wine stain).
Variations of closed angle glaucoma include pupillary block, aqueous misdirection and iridocorneal endothelial (ICE syndrome).