What is Macular Degeneration?
Age-related macular degeneration, commonly referred to as AMD, is a chronic condition that affects a person’s central vision. AMD is the cause of half of all blindness and severe vision loss in Australia, and it is estimated that 1 in 7 people over the age of 50 have signs of AMD. Yet, as it is a painless condition, they may not know it (MD Foundation). AMD generally affects both eyes, but one eye may be worse than the other.
It is believed that AMD arises from decades of aged-related oxidation causing gradual ageing damage to the photoreceptor cells, and to the supporting retinal pigmented epithelium (which normally replenishes the photoreceptors), as well as hardening of blood vessels reducing overall blood supply.
The macula area seems to be especially affected as it is the area of the highest photoreceptor density. This accumulated damage results in the build-up of waste products under the retina. They are seen macroscopically as yellow clumps called ‘drusen’ and are considered a hallmark sign of AMD if it occurs at the macula.
The damage leads to a change in the structure of the macula, resulting in central visual distortions or vision loss.
In simplistic terms, the macula accounts for your central vision, and is like a camera film that needs to be flat and dry to take a good picture.
In DRY AMD, the waterproof layer of the eye has blistered, so the vision becomes distorted.
In WET AMD, not only has the waterproof layer of the eye blistered, but it has also started to leak, and essentially, the eye cannot capture a sharp picture with a ‘soggy camera film’.
Diagnosing AMD
An eye specialist (Optometrist or Ophthalmologist) will need to do a comprehensive eye exam to diagnose AMD.
As a guide, if you are over 50, it is recommended you have an eye exam to check your macula at least every 2 years. If you are 65 or older, the recommendation is an eye exam every year.
However, your eye specialist will advise how often you should get your macula checked depending on your individual circumstances and whether you have a higher risk of developing AMD.
Some common tests that may be done by your eye specialist to provide a more complete clinical picture of your eye and help determine the type, location, and extent of any retinal condition, include:
To make a diagnosis of AMD, your Ophthalmologist will take your eye history and conduct a comprehensive eye examination. It is likely that your pupils will be dilated (with drops that blur your reading vision for 2-3 hours) to allow for a better examination of the inside of your eye.
An optical layered scan of the retina which can assist in the diagnosis and treatment monitoring of many retinal conditions, including AMD. An OCT scan uses light to produce very high-resolution cross-sectional images of the layers of the retina. OCT scans are also used to monitor your individual response to any treatment you have.
A non-invasive retinal imaging tool effective in the early detection of some retinal conditions as it highlights a retinal pigment (lipofuscin) which increases with retinal damage.
If your eye specialist suspects you have wet (neovascular) AMD, an ophthalmologist may perform a fluorescein angiogram which involves injection of a coloured dye (fluorescein) into a vein in the arm, followed by specialised photography of the retina through a dilated pupil. The dye highlights retinal blood vessels to shine brightly (“fluoresce”) under a special light, and this test helps identify abnormal blood vessels and retinal changes to allow diagnosis and treatment.
Allows examination of blood flow within the choroid and retina.
The Different Types of AMD
There are two main types of late-stage age-related macular degeneration:
Dry AMD is a gradual and progressive degeneration of the light-sensitive photoreceptors located at the macula, reducing central vision.
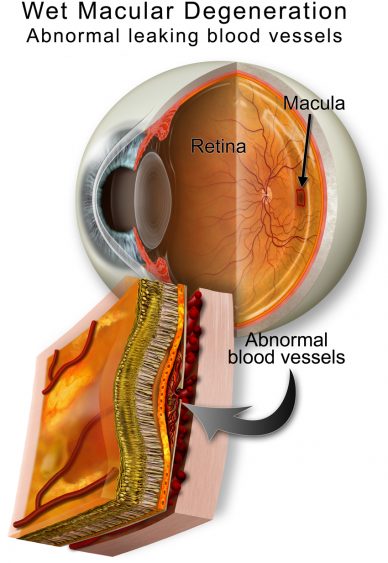
Wet (neovascular) AMD occurs when there is development of abnormal and highly fragile blood vessels (neovascularization) under the retina that leak or bleed into the retina and result in a rapid reduction and distortion of vision.
Dry AMD
Dry age-related macular degeneration (AMD) is the most common form of macular degeneration, and it can go unnoticed as it slowly and painlessly progresses over a longer period.
The retinal pigment epithelial (RPE) cells atrophy (slowly die), which in turn results in the gradual loss of photoreceptors and thinning of the macula. Dry AMD results in gradual distortions and decline in central vision, while peripheral vision remains relatively unaffected.
AMD can be classified by the size of drusen, from early, intermediate to advanced. However, it does not necessarily correlate with the extent of visual loss.
Wet (neovascular) AMD
As age-related macular degeneration (AMD) advances from early, intermediate to late stages, it can also progress from dry to wet AMD.
Wet AMD is the most aggressive form of AMD, and without intervention can cause rapid and permanent vision loss. It is characterized by the development of abnormal and highly fragile blood vessels (neovascularization) under the retina that can leak fluid or bleed into the macula, often at places where drusen deposits are formed.
These changes can result in a rapid loss of central vision, and variable recovery depending on when treatment is started.
Specialist Treatment for Macular Degeneration
Consultations with our specialists are available at three convenient clinic locations across the Gold Coast, fully equipped for the diagnosis, treatment and management of all eye-related conditions.