Overview
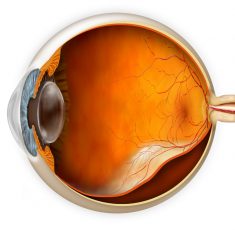
Retinal problems, conditions, and diseases can affect different parts of the retina and the impact on a person’s vision can range between being mildly affected to blindness.
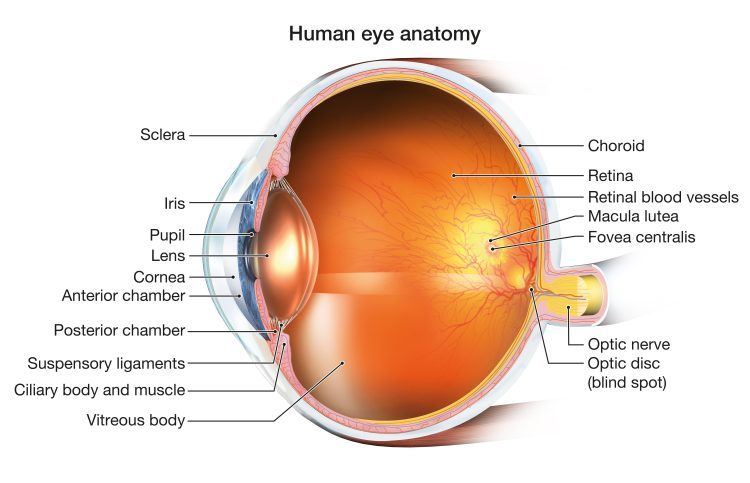
The retina is the inner layer of the eye containing photoreceptor cells, support cells and ganglion cells, which form the tracts for the optic nerve in an organised structure. The retina converts light into a signal that is conveyed to the brain through the optic nerve. The brain then interprets these signals and creates the image that we “see”.
Treatment is available for some retinal problems and depending on your condition, treatment goals may be to stop or slow vision loss, or to restore vision. Left untreated, some retinal conditions such as a Retinal Detachment can cause severe vision loss or blindness.
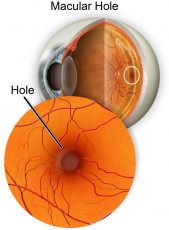
Macular Hole
As we age, the vitreous, a jelly-like substance that fills your eye and gives it its shape, will become watery and can collapse towards the centre of your eyeball. If the vitreous is firmly attached to the macula (part of the retina at the back of the eye), it can pull on it, causing a small tear or hole.
Your macula is the part of the eye responsible for your sharp, central vision. If left untreated, a macular hole can enlarge over time causing your central vision to blur and deteriorate, while peripheral vision remains normal.
Most macular holes require surgery and there are two main stages to the treatment.
Vitrectomy surgery to remove the vitreous and insert a gas bubble into the eye to support its structure.
Recovery period when the gas bubble pushes the retina back into place and closes the hole (the gas will be absorbed as the eye naturally refills with vitreous fluid).
The longer you have had a macular hole, the more difficult it is to recovery lost vision, which is why it’s important to see a specialist within weeks rather than months.
Read more about vitrectomy surgery and the symptoms of macular holes.
Retinal Tears and Retinal Detachments
A Retinal Detachment occurs when the inner layers of the retina separate from the underlying supportive tissue that provides its oxygen and nutrients.
A retinal detachment is an ocular emergency that can cause permanent vision loss and you should seek urgent medical attention. Eye Specialist Institute provides access to ophthalmic care for emergency after-hours and weekend appointments. Call us on 1800 RETINA (1800 738 462).
The impact on a person’s eyesight depends on the location and severity of the detachment and symptoms can include:
- o Sudden onset of new floaters often appears as dark dots, specks, cobwebs or squiggly lines in vision
- o Bright flashing lights or sparks (like lightning or a camera flash) in your side vision
- o Dark shadow or grey curtain obscuring your side vision
- o Blurred or decreased vision
- o Complete and sudden loss of vision
The aim of retinal detachment surgery is to halt the progression of vision loss by reattaching the retina to the back of the eye. The type of surgery recommended for your retinal detachment will depend on the cause, location, and type of detachment as well as any existing eye conditions.
Read more about what can cause retinal tears and detachments, and treatment options.
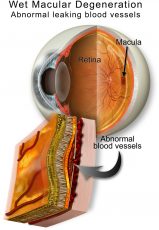
Macular Degeneration
Macular Degeneration, commonly referred to as age-related macular degeneration, is a condition that affects a person’s central vision due to the deterioration of the central retina.
Central retinal deterioration often occurs with ageing, and there are two main types of age-related macular degeneration (ARMD):
Dry ARMD is a gradual and progressive degeneration of the light-sensitive photoreceptors located at the macular, slowly reducing vision.
Wet (neovascular) ARMD is the development of abnormal and highly fragile blood vessels under the retina that leak or bleed resulting in a rapid reduction and distortion of vision.
While anyone can develop age-related macular degeneration, several factors can place you at greater risk including being over 40, having a family history of macular degeneration, and high myopia. Read more about macular degeneration risk factors and treatment options.
There is useful self-check tool, that you can use at home to monitor changes in your vision called an Amsler grid which is a card that shows a grid pattern with a dot in the centre. You can contact us for your free Amsler grid (with a magnet on the back so you can stick it to your fridge) on 1800 111 374 or download a copy here.
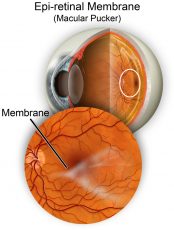
Epiretinal Membrane
An Epiretinal Membrane, or macular pucker, is thin layer of tissue that has formed over the retina. Over time these cells contract and form scar-tissue which can pull and distort the shape of the macula resulting in blurry and ‘wavy’ central vision.
In many cases, the symptoms of vision distortion and blurriness are mild, so no treatment is necessary although regular monitoring is advised.
Vitrectomy surgery may be recommended if an epiretinal membrane progresses to cause significant vision deterioration that affects daily activities.
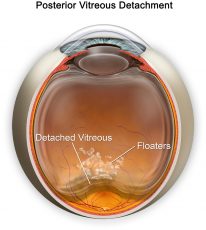
Posterior Vitreous Detachment
A Posterior Vitreous Detachment or PVD is a natural and common occurrence with age and happens when the vitreous gel begins to shrink and eventually separates from the retina.
The most common symptom of PVD is blurred vision from a sudden increase or change in floaters which often appear as dark dots, specks, cobwebs or squiggly lines that move across your field of vision. You may also notice flashes like lightning or a camera flash in your peripheral vision.
Unlike a migraine, this occurs in one eye at a time.
These symptoms will usually settle down over about two months. Though the perception of floaters will improve over this time, they will never completely disappear. Most people are not too bothered, but some are, depending on where the floater settles relative to the visual axis. If bothersome, the floaters can be eradicated – speak to your vitreoretinal surgeon about this.
However, as symptoms of a PVD can mimic those of a more serious sight-threatening conditions such as retinal detachment, you should schedule an eye exam with your Optometrist or Ophthalmologist for a full examination with pupil dilation within 3-4 days to ensure no other issues are present.
Read more about the causes and treatment options for a posterior vitreous detachment.
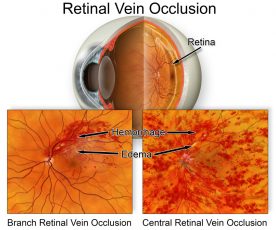
Retinal Vein Occlusion
A Retinal Vein Occlusion (RVO) is when a vein becomes occluded and can cause a backflow of blood in the retina and the resulting disruption to the blood supply causes vision related complications.
They are characterised by the extent of involvement of the retinal vein.
Affects the central retinal vein close to the optic nerve, resulting in poor blood flow throughout the entire retina and can cause severe vision loss and complications like neovascular glaucoma.
Affects a further branch of retinal vein and can result in a variable loss of vision.
Venous occlusions are associated with high blood pressure, diabetic retinopathy and can have complications of glaucoma.
Treatments are aimed at minimizing the complications from the retinal vein occlusion to decrease the risk of further vision loss and/or pain. There is no treatment currently to reverse the retinal vein occlusion.
Anti-VEGF (Anti-Vascular Endothelial Growth Factor) injections shrink the abnormally leaky blood vessels causing neovascular glaucoma and allow resorption of visually significant excess retinal fluid (macular oedema). This medication is administered via intravitreal injection.
Retinal laser photocoagulation can also be used to reduce leaky blood vessels and persistent excess retinal fluid.
Vitrectomy surgery may be recommended in some cases, complicated by vitreous haemorrhages.
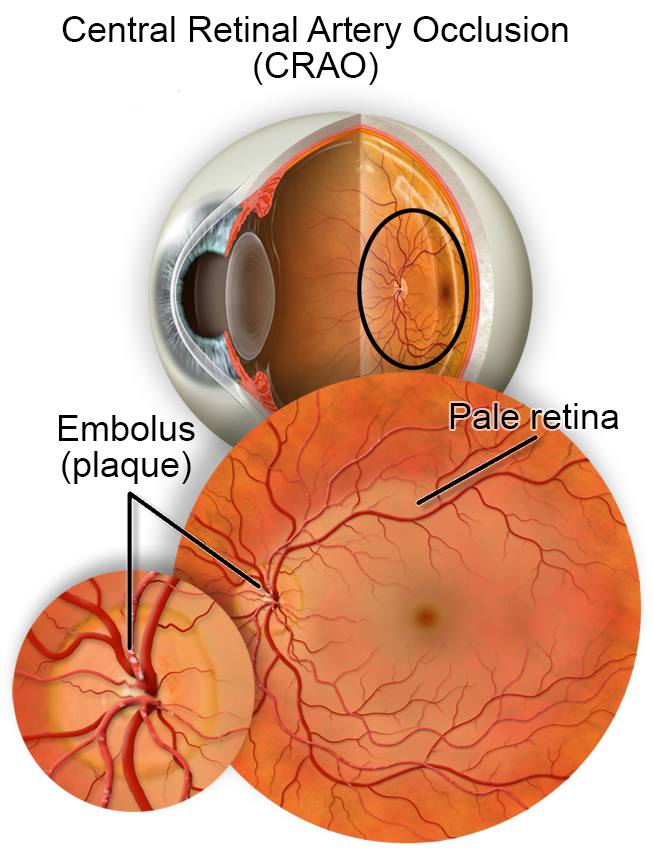
Retinal Artery Occlusion
A Retinal Artery Occlusion is a blockage of the artery supplying blood flow to the artery in the retina and can result in sudden, severe painless vision loss to one eye.
They are also characterised by the extent of involvement of the retinal artery.
Affects the central retinal artery close to the optic nerve, resulting in poor blood flow throughout the entire retina and often results in full loss of vision.
Affects a further branch of retinal artery and can result in a variable loss of vision.
This is a medical emergency that can cause permanent vision loss and can be a precursor disease to strokes. Some cases can also be related to giant cell arteritis, and early treatment is crucial to prevent loss of vision in the other, seeing eye.
Seek immediate medical attention as timely investigations and treatments may reverse some vision loss and prevent further complications. Contact ESI on 1800 RETINA (1800 738 462).
Read more about the symptoms and causes of a retinal artery occlusion.
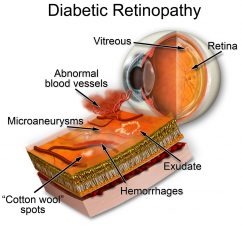
Diabetic Retinopathy
Diabetic Retinopathy is a serious, sight-threatening disease that affects the blood vessels inside the retina. It is the most common form of blindness in Australians under the age of 50 and is commonly associated with poor blood glucose control.
When the blood vessels are damaged, they are unable to deliver oxygen and nutrients to retinal tissue, which is needed to maintain good vision.
The danger with diabetic retinopathy is that there are no early-stage signs and late-stage symptoms include:
- o Blurred or distorted vision that makes it difficult to read, watch television or recognise faces
- o Increased sensitivity to glare and difficulty seeing at night
- o Eye strain and headaches
The severity of this disease can also be intensified due to smoking, high cholesterol levels, and high blood pressure.
Regular eye examinations and treatment can help to maintain your vision however there is unfortunately no cure for diabetic retinopathy.
Read more about the three main types of diabetic retinopathy and treatment options.
Central Serous Retinopathy
Central Serous Retinopathy, or CSR, is a condition where fluid leaks under the retina, causing a fluid-filled (serous) detachment and vision distortion or loss.
It is most often confined to the macula, which is the part of the retina responsible for detailed central vision.
In most cases, CSR will resolve within one to four months without treatment, as the fluid is reabsorbed. However, recurrences are common, and some symptoms may persist, including distortions, reduced contrast sensitivity and dullness of colours.
In cases where the fluid does not reabsorb on its own, a fluorescein angiogram may be used to identify the site of leakage.
Treatment involves photodynamic therapy (PDT) with verteporfin (Visudyne) as a photosensitizing agent. This specialised laser treatment allows targeted sealing of affected blood vessels and may be repeated for recurrences. Green laser can be used in select cases, if the focus of leakage is away from the fovea.
Read more about what causes central serous retinopathy, CSR, and how it is diagnosed.
Access Expert Treatment for Retinal Problems on the Gold Coast
Consultations with our specialists are available at three convenient clinic locations across the Gold Coast, fully equipped for the diagnosis, treatment and management of all eye-related conditions.