What is the retina?
The retina is the inner layer of the eye containing photoreceptor cells, support cells and ganglion cells, which form the tracts for the optic nerve in an organised structure.
The retina is responsible for collecting optical information and the optic nerve is then responsible of sending that visual information to the brain.
There are two different types of photoreceptors (“pixels”) located in the retina – these are called rods and cones:
- - Rod photoreceptors detect motion, provide black-and-white vision and function well in lower light.
- - Cone photoreceptors are work best for fine acuity, colour vision and perform best in medium/bright light.
Rods are located across the retina, whereas cones are concentrated in a specific central area called the macula.
What is the function of the retina?
The retina converts light into a signal that is conveyed to the brain through the optic nerve. The brain then interprets these signals and creates the image that we “see”.
What is the macula?
The macula is the optical centre of the retina and is approximately 5mm wide. It is primarily responsible for our fine acuity (reading) and colour vision.
At the centre of the macula there is a small dip called the fovea which is about 1.5mm wide and contains only tightly packed cone photoreceptors without any impeding nerves or blood vessels, important for its function of fine detail vision.
What are floaters and flashes in my eye and are they a bad sign?
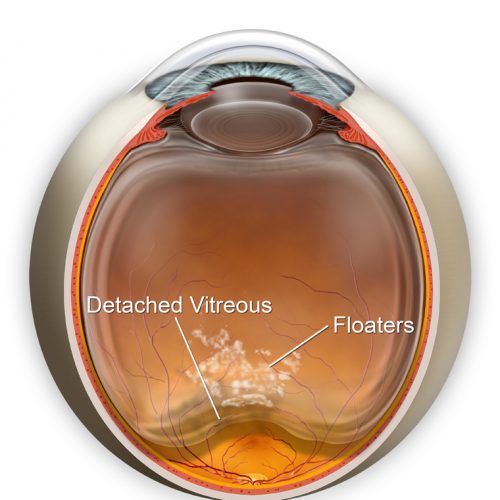
Floaters are commonly caused by the shrinking of the vitreous gel inside the eye, flashes occur as a result of mechanical pulling of the vitreous gel on the retina. When this process occurs naturally with ageing, it is known as a Posterior Vitreous Detachment (PVD).
Unfortunately, the symptoms can simulate those seen in retinal tears or detachment, and therefore it is recommended that the sudden onset of new floaters and flashes should warrant an eye specialist review within 3-4 days to 1 week to rule out these sight threatening conditions.
In most cases, Posterior Vitreous Detachment symptoms will improve over time.
What are some common retinal problems?
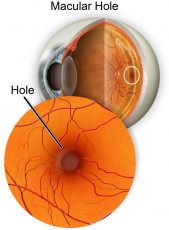
As we age, the vitreous gel can shrink and pull towards the centre of your eyeball. In some people, the vitreous gel is firmly attached to the macula and this pull can lead to the structurally weak macula to open up into a partial hole (lamellar hole) or full thickness hole.
This hole may result in a central blind spot or waviness in vision. If left untreated, a macular hole can enlarge over time causing increasing central blindness, while peripheral vision remains normal.
Macular Holes require surgery to fix, and often requires a period of posturing with gas to ensure full closure of the hole – read more about vitrectomy surgery and macular holes.
Think of the retina like a ‘wallpaper’ attached to inner shell of the eye.
A retinal tear occurs when a break in the ‘wallpaper’ forms. If the ‘wallpaper’ is still attached on the wall of the eye, the tear can be sealed off with a laser procedure, mitigating the need for an operation.
A retinal detachment occurs when intraocular fluid has gone under a retinal tear, ripping the ‘wallpaper’ off the wall. A retinal detachment is an ocular emergency that can cause permanent vision loss. You must seek urgent medical attention.
The aim of retinal detachment surgery is to halt the progression of vision loss by reattaching the retina to the back of the eye –read more about retinal tears and detachments.
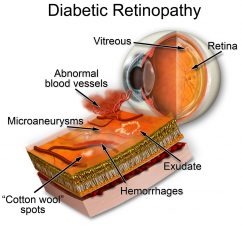
Diabetic retinopathy is a serious and sight-threatening disease that affects the blood vessels inside the retina. It is the most common form of blindness in Australians under the age of 50, with duration of diabetes and less-optimal control of diabetes major risk factors.
Diabetic retinopathy occurs as a result of oxidation damage to blood vessels due to high blood glucose. This results in a reduced ability to deliver oxygen and nutrients to retinal tissue and can lead to formation of malformed blood vessels which often leak blood into the retina.
These factors can lead to permanent injury to the highly metabolic tissue of the retina and can even result in sequelae such as retinal detachment, cataracts, and macular oedema, all of which can cause a reduction in vision.
Mild to moderate grades of diabetic retinopathy are managed with close observation and optimizing control of blood glucose levels, whilst severe or proliferative grades can require retinal laser or intravitreal injections – read more about the three main types of diabetic retinopathy.
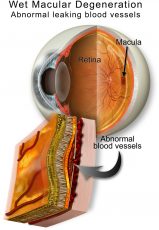
Macular degeneration, commonly referred to as age-related macular degeneration (ARMD), affects the central vision.
It occurs as a result of accumulation of waste products and oxidation damage to the supporting tissue layer of the retina, the retinal pigmented epithelium (RPE). As this layer becomes damaged, the photoreceptors will also become irreversibly damaged.
There are two main types of age-related macular degeneration (ARMD):
– Dry ARMD is a gradual and progressive degeneration of the light-sensitive photoreceptors located at the macula, slowly reducing vision.
– Wet (neovascular) ARMD is the development of abnormal and highly fragile blood vessels under the retina that leak or bleed resulting in a rapid reduction and distortion of vision.
Treatment is required urgently and usually consists of intravitreal injections with medications designed to stabilise these leaky blood vessels.
While anyone can develop age-related macular degeneration, several factors can place you at greater risk – read more about macular degeneration risk factors and treatment options.
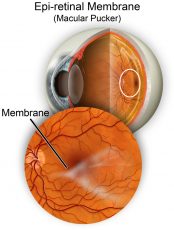
An Epiretinal Membrane, or macular pucker, is thin layer of tissue that has formed over the macula. Over time these cells contract, pull and crinkle the macula, which result in blurry and ‘wavy’ central vision.
In many cases, the symptoms of vision distortion and blurriness are mild, so no treatment is necessary although regular monitoring, especially with a Amsler grid chart, is advised.
Vitrectomy surgery may be recommended if an epiretinal membrane progresses quickly or cause significant vision deterioration – read more about epiretinal membrane symptoms and causes.
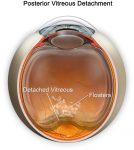
A Posterior Vitreous Detachment or PVD is a natural and common occurrence with age and happens when the vitreous gel begins to shrink and eventually separates from the retina.
The most common symptom of PVD is blurred vision from a sudden increase or change in floaters which often appear as dark dots, specks, cobwebs, or squiggly lines that move across your field of vision. You may also notice flashes like lightning or a camera flash in your peripheral vision.
Unlike a migraine, this occurs in one eye at a time.
These symptoms will usually settle down over about two months. Though the perception of floaters will improve over this time, they will never completely disappear. Most people are not too bothered, but some are, depending on where the floater settles relative to the visual axis. If bothersome, the floaters can be eradicated – speak to your vitreoretinal surgeon about this.
However, as symptoms of a PVD can mimic those of a more serious sight-threatening conditions such as retinal detachment, you should schedule an eye exam with your Optometrist or Ophthalmologist for a full examination with pupil dilation within 3-4 days to ensure no other issues are present – read more about the causes and treatment options for a posterior vitreous detachment.
Read more about other retinal conditions, including, Retinal Vein Occlusion, Retinal Artery Occlusion, and Central Serous Retinopathy.
What are the symptoms of retinal problems?
Retinal diseases and conditions can affect different parts of the retina and the impact on a person’s vision can range between being mildly affected to blindness.
Some retinal diseases can share several similar symptoms which may include:
- seeing flashes of light
- a sudden onset of floaters
- changes in or loss of central or side (peripheral) vision
- blurry, dark, or empty spaces in field of vision (scotoma)
- reduced intensity or brightness of colours
- difficulty seeing at night
- trouble adjusting to low light levels
Many of these symptoms could indicate more serious sight-threatening conditions and you should seek specialist advice to the significance of these, especially if they have occurred suddenly.
Why do I need surgery for a retinal detachment?
A retinal detachment is a serious condition that is considered an ocular emergency and requires prompt surgical management as it can potentially lead to blindness.
The aim of surgery is to halt vision loss by reattaching the retina to the appropriate support structures.
Generally, the sooner the retina is reattached, the better the chances that vision can be maintained or restored.
The type of surgery recommended by your Ophthalmologist will depend on the cause, location, and type of detachment as well as any existing eye conditions.
Can I self-check my retina and macula?
Regular comprehensive eye exams with an Optometrist or Ophthalmologist provides the best protection for identifying retinal conditions. This involves your eyes being dilated (with drops that blur your reading vision for 2-3 hours) to allow for a better examination of the back inside of your eye.
A useful self-check tool that you can use at home to monitor changes in your central vision for macular diseases is an Amsler grid which is a card that shows a grid pattern with a dot in the centre.
You can contact us for your free Amsler grid (with a magnet on the back so you can stick it to your fridge) on 1800 111 374.You can also download and print a paper copy here.
To use your Amsler grid:
- Wear your reading glasses or contact lenses and hold the chart at a comfortable reading distance (approx. 30cm).
- Cover one eye and focus on the black dot in the middle of the grid.
- Swap sides and repeat the test with the other eye.
- If the lines appear to be distorted (wavy, broken, dim, or fuzzy), or there are blurred or dark patches on the grid – schedule an eye exam immediately.
While the Amsler grid is a quick sight test that you can do daily, you should not rely on it for diagnosis, and we recommend you pair your daily self-checks with regular eye examinations with your Optometrist or Ophthalmologist.
Speak with your eye specialist as a matter of urgency if you notice any sudden changes, including:
- sudden loss of vision in one eye
- sudden hazy or blurred vision
- dark curtain-like blotting out of part of vision
- sudden or increased flashes of light or black spots
- loss of peripheral (side) vision
Eye Specialist Institute provides access to ophthalmic care for emergency after-hours and weekend appointments. To contact us in the event of an ocular emergency phone 1800 RETINA (1800 738 462).
How are retinal problems diagnosed?
To make a diagnosis of a retinal condition your Ophthalmologist will take your eye history and conduct a comprehensive eye examination. It is likely that your pupils will be dilated (with drops that blur your reading vision for 2-3 hours) to allow for a better examination of the inside of your eye.
Some common tests that may be done by your eye specialist to provide a more complete clinical picture of your eye and help determine the type, location, and extent of any retinal condition, include:
An optical layered scan of the retina which can assist in the diagnosis and treatment monitoring of many retinal conditions and glaucoma.
A non-invasive retinal imaging tool effective in the early detection of some retinal conditions as it highlights a retinal pigment (lipofuscin) which increases with retinal damage.
Involves injection of a coloured dye (fluorescein) into a vein, and specialised photography of the retina through a dilated pupil. The dye highlights retinal blood vessels to shine brightly (“fluoresce”) under a special light, and this test helps identify abnormal blood vessels and retinal changes to allow diagnosis and treatment.
A non-invasive tool that uses soundwaves to help view the status of the retina, especially if there is obscuration of retinal view by a vitreous haemorrhage.
Specialised radiological testing may be ordered by your Ophthalmologist in certain cases.
Allows examination of blood flow (but not leakage) within the choroid and retina
What can I do to protect the health of my retina?
- Eat a healthy and balanced diet with a variety of brightly coloured fruits and vegetables, along with antioxidant supplements if recommended by your specialist to minimise oxidative damage.
- Wear a pair of good quality sunglasses and a wide-brimmed hat to minimise UV damage
- Stop smoking and limit alcohol consumption
- Find physical activities you enjoy and maintain a healthy weight
- Manage your blood pressure and diabetes (if you have it)
- Take safeguards to reduce the risk of a trip or fall causing eye injuries – it can happen to anyone
- Get regular dilated eye examinations for early diagnosis and treatment of eye conditions
- Be an advocate for your health – you can ask for a referral to see a specialist of your choice. Download a referral form to take to your GP or Optometrist.
- Don’t ignore changes in your vision – a sudden increase in floaters, flashes, or a dark curtain can all indicate a serious sight-threatening eye condition that needs urgent attention
- Read more about looking after your eye health at any age